Cranial cruciate ligament injuries are the most common culprits for hind limb lameness in canine patients. What may appear as a sudden injury, many CCL ruptures are in fact a result of slow degeneration/weakening of the CCL.1 It is proposed that therapeutic intervention during those early stages of degeneration could result in the healing and repair of the ligament, potentially negating (or at least delaying) the need for surgical intervention. In this blog post, we will explore the treatment options for CCL injuries and the potential use of regenerative medicine as a treatment for early partial tears.
The Cranial Cruciate Ligament (CCL)
The cranial cruciate ligament is one of four major ligaments in the canine stifle. It is responsible for maintaining stability of the stifle by preventing the tibia from excessive movement, hyperextension of the stifle, internal rotation and it also aids in proprioception (the animal’s awareness of placement of the limb). The CCL is the most common ligament injured in the canine patient, accounting for the majority of orthopedic conditions seen in the veterinary practice.
Diagnosing CCL Injuries
Typically, the patient with a suspected CCL injury will present a history with one or more of the following signs/symptoms1:
- Difficulty rising from a sit
- Trouble jumping into the car
- Decreased activity level
- Lameness (limping) of variable severity
- Muscle atrophy (decreased muscle mass in the affected leg)
- Decreased range of motion of the knee joint
- A popping noise (which may indicate a meniscal tear)
- Swelling on the inside of the shin bone (fibrosis or scar tissue)
- Pain
- Unwillingness to play
- Stiffness
During examination, veterinarians may employ several diagnostics to confirm rupture of the ligament including palpation, radiographs and synovial fluid testing (to rule out other joint related diseases).
Treating the Fully Ruptured CCL
When a CCL has fully ruptured (or torn), surgical intervention is commonly recommended to correct the instability and to return function back to the joint. While no single surgical procedure has been established as the superior method, techniques that are often employed include Tibial Plateau Leveling Osteotomy (TPLO), Tibial Tuberosity Advancement (TTA), Tightrope and lateral suture. Typical surgery costs may range from $1,000 to $5,000, or more. Whether or not the patient undergoes surgery, there is a high probability that the arthritis will develop within the joint and there is a 40-60% chance the opposite CCL will rupture in the future.
The Challenges of Partially Torn CCL’s
1. Diagnosis
While the above mentioned diagnostics are usually sufficient in confirmation of a complete CCL rupture, partially torn CCL’s can be challenging to diagnose due to inconclusive palpation findings and presence of stability in the joint. For these patients, diagnosing the partially torn ligament may require additional diagnostic capabilities such as arthroscopy (or needle scope) or further investigation into the patient’s lameness history if no other diagnostics are available.
2. Treatment
For the completely torn CCL, surgical interventions are necessary to stabilize the joint and prevent further damage if possible. But what about the partially torn CCL?
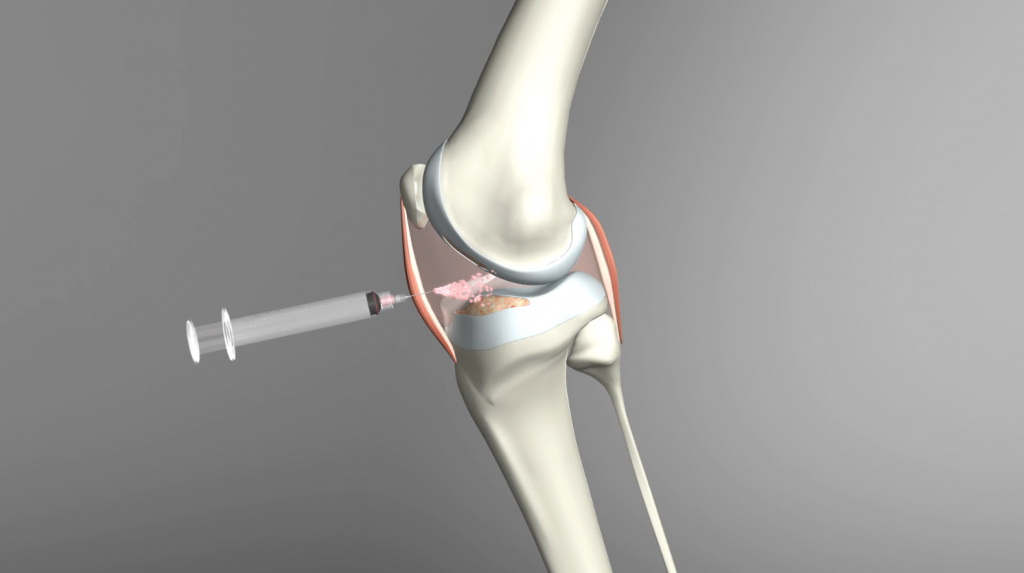
Current treatment options geared towards the partial CCL tear are focused on pain management and limb stabilization. While both are needed for recovery and repair of the tissue, the repair of the cruciate ligament is limited by the vascularization of the tissue and the number of cells that are needed to repair the damage.
Although surgery can provide the stabilization needed for the joint, it is an invasive procedure not without some risks to the patient. What if the stability of the joint is not yet compromised? If the joint still has some form of stability and the ligament is in the early stages of degeneration, can the joint be treated in a minimally invasive manner to prevent further injury and repair the tissue?
In one recently published study, these questions were investigated and the use of regenerative medicine for the treatment of partial CCL tears was examined.2
Regenerative Medicine for the Treatment of Partial CCL Tears
In this retrospective analysis, investigators reviewed the records of 36 client-owned canines that had a unilateral, partially torn CCL (defined as less than 50% tear in their CCL’s) and were treated with a combination of stem cells (adipose or bone marrow derived) and platelet rich plasma in combination with rehabilitation therapy and a functional stifle brace. The study investigated the patients’ pressure index, collected pet owner surveys and performed 90 day follow up arthroscopic examinations on 13 out of the 36 original study patients.
Results of the study were promising with 10 out of the 13 patients having fully intact CCL’s visualized on 90 day follow up arthroscopy with neovascularization and normal fiber pattern. 3 out of the 13 patients had progressed to more than 50% tear or completely ruptured, in which case a TPLO was performed. When owners were asked about their pets’ recoveries, all respondents believed their dog had excellent or very good quality of life and their dogs’ recovery was excellent or good.
Return of the Athlete?
This study not only looked at “weekend warriors” but also the high-level athlete. Seven (7) of the dogs that were observed in this study were designated as performance dogs and at the conclusion of the study, 6/7 dogs had returned to sport. Of the six that returned to sport, four patients were back to competing at the same level and two were back to competing at a higher level.
What Conclusions Can We Draw from This Study?
Even with certain study limitations, the results from the available patients showed a promising possible alternative to treating an injury that may have otherwise resulted in a full rupture. From this data, one may hypothesize that if partial CCL injuries are detected early in their development and are treated with a combination approach of platelet rich plasma and stem cell therapy, there is a chance that the ligament could heal, negating the immediate need for surgical intervention. This could not only improve the patient’s quality of life, but also provide a minimally invasive therapeutic alternative.
While surgery will always have its place in CCL rupture recovery, perhaps it’s not the only tool in the toolbox available for small animal practitioners.
To be the first to know when new studies, education webinars, articles, and blog posts like these are published, make sure you sign up for our monthly newsletter: http://www.litecureinfo.com/CompanionWellnessReportOptIn
References:
1. Cranial Cruciate Ligament Disease, www.acvs.org/small-animal/cranial-cruciate-ligament-disease
2. Canapp SO Jr, Leasure CS, Cox C, Ibrahim V and Carr BJ (2016). Partial Cranial Cruciate Ligament Tears Treated with Stem Cell and Platelet-Rich Plasma Combination Therapy in 36 Dogs: A Retrospective Study. Front. Vet. Sci. 3:112. Doi:10.3389/fvets.2016.00112
Have you heard of the term “prolotherapy” and wondered: “Is that the same as platelet rich plasma or stem cell therapy?”. If you answered “yes”, you’re not alone! Prolotherapy, also known as “proliferation therapy” or “regenerative injection therapy”, is a term that is used to describe an area of therapeutics that result in proliferation and healing of damaged tissues.
Sounds very familiar to regenerative medicine, doesn’t it? That’s because prolotherapy works under the same principal of utilizing the body’s own healing capabilities to heal and repair tissues. But what makes it different than platelet rich plasma and stem cell therapies? In this blog, we will explore the uses of prolotherapy, what it consists of and how it differs in its method of action from the regenerative therapies we have come to understand.
What is prolotherapy?
Prolotherapy is a therapy in which an irritant solution is injected at a site of injury/pain with the goal of eliciting a temporary, low grade inflammatory response resulting in healing and repair of connective tissues. The irritant typically used for these procedures consists of 12-25% of Dextrose, the naturally occurring form of glucose.
How does prolotherapy work?
It is generally accepted that when a solution consisting of more than 10% dextrose is injected into a tissue, it creates an osmotic gradient outside of the cells. When a prolotherapy solution is injected into the tissue, it draws out water from within the cells, resulting in their lysis, also described as osmotic shock. When cells undergo apoptosis, they release signals to the body to undergo a wound-healing cascades at the specific sites of injuries. In essence, prolotherapy creates a minor injury to the tissue with the goal of an increased healing response to the tissue.1
What is prolotherapy typically used for?
Prolotherapy has been reported to be useful in facilitating the repair of weakened or unstable tendons and ligaments as well as various forms of spinal pathologies resulting in pain. While numerous studies have attempted to investigate prolotherapy for use in osteoarthritis, there has been very little evidence showing its efficacy over placebo for outcomes surrounding pain, peak vertical force, and range of motion in enrolled canine patients.1
How does prolotherapy differ from platelet rich plasma and stem cell therapies?
While prolotherapy does elicit an inflammatory response resulting in growth factors and healing cascades, it requires injecting an irritating solution to produce such a response. This irritating solution can be painful during and after the injection, necessitating an anesthetic agent to be utilized in conjunction with the injection.
In platelet rich plasma and stem cell therapies, the body’s own cells are injected into the site of injury where they initiate the healing cascade at the affected tissue. The environment of the tissue is modulated through naturally occurring pathways facilitated by the cells being injected. Since platelet rich plasma and stem cell therapies utilize the body’s own cells and the injection of them creates minimal irritation, further damage of the tissue is avoided.
References 1. J. Matthew Sherwood, James K. Roush, Laura J. Armbrust, and Walter C. Renberg (2017) Prospective Evaluation of Intra-Articular Dextrose Prolotherapy for Treatment of Osteoarthritis in Dogs. Journal of the American Animal Hospital Association: May/June 2017, Vol. 53, No. 3, pp. 135-142.What purpose do resident stem cells serve in the body? This is a fair but yet complicated question as our knowledge has only reached the “tip of the iceberg” with stem cell biology. Previously we have discussed adult stem cells, their use as a therapy, and made mention of the recruitment of resident stem cells to a site of injury. But what do we know about the stem cells that reside in the numerous tissues of the body? In today’s blog, we will explore the current scientific knowledge of resident stem cells, what they do (and do not do) and uncover some little facts that might even surprise you!
1. What are resident stem cells?
Every individual (both two legged and four legged) has stem cells residing in their tissues and organs. Also referred to as adult stem cells, these cells are characterized by two very important attributes1:
1. Self- renewal: the ability to divide without differentiation
2. Multipotency: the capacity to specialize in different cell types
2. Where can these resident stem cells be found?
Almost every tissue in the body has resident stem cells housed in what is called a “stem cell niche”. This niche is generally understood to be a “micro-environment” where stem cells reside and where they receive signals from other cells in the body to activate, self-renew or remain dormant2.Stem cell niches can be equated to an operator providing assistance. They receive “calls” from the tissue, direct the message to the appropriate “department” (stem cell) and determine the action that is needed for resolution (“pick up the call”-stem cell to activate/ differentiate, “set up meeting”- self renew or “send to voicemail”- stay dormant).
- Bone Marrow
- Adipose
- Brain
- Peripheral Blood
- Blood Vessels
- Skeletal Muscles
- Skin
- Teeth
- Hair
- Gut
- Liver
- Reproductive Tissues
3. What purpose do resident stem cells serve in the body?
The primary role of resident stem cells is to maintain and repair the tissue in which they are found1. As discussed above, these stem cells are signaled through their niche to differentiate and respond to the area of damage.
4. Why are degenerative conditions and injuries treated with platelet rich plasma and stem cell therapies if resident stem cells are already present near the injured tissue?
Chronic conditions such as arthritis and DJD have a multitude of factors that contribute to the progression of the disease, many of which are beyond the scope of this blog. While stem cells may be located near the area of injury, there are several reasons why they may not be renewing the damaged cells in the tissue. Hypothesized reasons for this include:
1. Resident stem cells make up a very small number of cells in each tissue3. In the instance of a degenerative disease, the rate at which cells are replenished through resident stem cells can be suboptimal compared to what is necessary to fully repair the tissue. This constant demand for “repair mode” may also lead to the exhaustion of the regenerative potential of the tissue2.
2. As the body ages, so do the communication pathways between the tissues and the resident stem cells. These communication pathways, which are influenced by growth factors, can become disrupted or dysregulated, which can lead to slowed/halted renewal (stem cells stay dormant and/or limited in numbers) or unregulated production (ex. cancer)2.Regenerative medicine shows great promise in benefiting tissues where these communication pathways and imbalances are present. Platelet Rich Plasma provides beneficial growth factors which aid in the recruitment of resident stem cells while stem cell treatments have the potential to restore tissue homeostasis and structure.
5. What tissues have resident stem cells?
In the early days of research, few tissues were thought to have stem cells, which included bone marrow, fat, skin and muscle. Now, that list has grown exponentially to encompass1:
While more research is needed to fully understand the functions and purpose of resident stem cells, it is easy to see they are an important part of tissue biology and diseases. Stay tuned for our next blog where we will travel back in time to the early years of regenerative medicine!
1. NIH Stem Cell Information Home Page. In Stem Cell Information [World Wide Web site]. Bethesda, MD: National Institutes of Health, U.S. Department of Health and Human Services, 2016 [cited August 15, 2017] Available at < //stemcells.nih.gov/info/basics/7.htm>
2. Adv Exp Med Biol. 2010 ; 695: 155–168. doi:10.1007/978-1-4419-7037-4_11.
3. Adult mesenchymal stem cells and cell-based tissue engineering. R.S.Tuan, G. Boland and R.Tuli Arthritis Res Ther. 20025:32. https://doi.org/10.1186/ar614© BioMed Central Ltd 2003