As we continue to delve further into Platelet Rich Plasma and how it treats conditions, the most common questions that arise during discussions are:
- Do we want white blood cells in our PRP?
- If so, which white blood cells do we want to include?
In this post, we will explore the different types of white blood cells, their functions and whether they are beneficial or detrimental in Platelet Rich Plasma.
What are White Blood Cells?
White Blood Cells (WBCs), also known as Leukocytes, make up the majority of the body’s immune system. Their main purpose is to protect the body from foreign substances and various types of infections.
What are the different types of White Blood Cells?
- Neutrophils
- Monocytes
- Lymphocytes
- Eosinophils
- Basophils
What are their functions and are they beneficial when included in Platelet Rich Plasma?
1. Neutrophils
- Basic Function: Neutrophils are the first responders during an infection or injury. When there is a site of injury, they destroy germ cells through a process called phagocytosis, which in Ancient Greek literally means “to devour”. Neutrophils also kill invading cells through the release of reactive oxygen species and antimicrobial peptides which are toxic to the invading germ cells. 1
- Role in PRP: Neutrophils have been shown to release damaging molecules which can degrade collagen and other tissues along with extracellular matrix molecules. Neutrophils also release pro-inflammatory cytokines which leads to further damage in the tissue. Therefore, their inclusion in Platelet Rich Plasma, specifically for arthritic applications, is not recommended. 2
2. Monocytes
- Basic Function: The three main functions of monocytes are: phagocytosis, facilitation of communication between the innate and adaptive immune systems, and cytokine production.3
- Role in PRP: It has been found that Monocytes are associated with an increase in cellular metabolism and collagen production in fibroblasts. It has also been found that monocytes moderate the release of anti-angiogenic cytokines such as interferon-ɣ and IL-12.4 Therefore their inclusion in Platelet Rich Plasma is considered beneficial.
3. Lymphocytes
- Basic Function: Lymphocytes are the patrolling cells in the circulatory system that are responsible for recognizing and responding to invading pathogens. They are characterized into three subtypes: T-Cells, B-Cells and Natural Killer Cells (NKCs). T and B cell’s main function are to recognize pathogens and moderate the inflammatory response through the release of cytokines and antibodies. They also are accountable for adaptive immunity, meaning should the same pathogen be encountered again, the body is ready to respond with antibodies. Natural Killer Cells play a major role in defending the body from both tumors and virally infected cells. They are activated when cytokines (called interferons) are released, and produce cytotoxic granules that specifically destroy the altered cells.
- Role in PRP: Currently the significance of Lymphocytes in Platelet Rich Plasma unknown. It is known that platelets activate Lymphocytes as part of the healing cascade through elevated levels of IL-6, however their benefit or detriment to PRP is still unclear.
4. Eosinophils
- Basic Function: Eosinophils are most commonly known as a defense mechanism against parasites and are important mediators of allergic reactions.
- Role in PRP: Eosinophils are known to produce several beneficial growth factors including VEGF, PDGF and TGF-β. These growth factors are associated with angiogenesis, cellular proliferation and extracellular matrix formation.5 Therefore their inclusion in Platelet Rich Plasma may be beneficial in tissue repair.
5. Basophils
- Basic Function: Basophils are also recognized to play a role in parasite defense and allergic reactions. They release several proteins that increase vascular permeation and regulation of the inflammatory process.
- Role in PRP: The role of Basophils for PRP are relatively unknown. Basophils are known to secrete pro inflammatory cytokines but little is known if these are beneficial or detrimental to a PRP sample.
What is the bottom line?
With the current knowledge and research surrounding White Blood Cells, it is generally understood that a PRP sample should include an increase in Monocytes and a decrease in Neutrophils. Knowledge regarding the role of Lymphocytes, Eosinophils and Basophils in PRP is still limited, therefore absolute decisions on their inclusion or exclusion cannot be made. But as our understanding of White Blood Cells and their roles in PRP continue to evolve, formulations of PRP in the future may change to treat a specific condition, moving this from a personalized medicine to a precision medicine.
Stay tuned for our next blog where we will answer your questions about Platelet Rich Plasma. To submit a question for our next blog, email heatherw@companiontherapy.com.
References:
- Mayadas, T. N., Cullere, X., & Lowell, C. A. (2014). The Multifaceted Functions of Neutrophils. Annual Review of Pathology, 9, 181–218. http://doi.org/10.1146/annurev-pathol-020712-164023
- Helen L. Wright, Robert J. Moots, Roger C. Bucknall, Steven W. Edwards; Neutrophil function in inflammation and inflammatory diseases. Rheumatology (Oxford) 2010; 49 (9): 1618-1631. doi: 10.1093/rheumatology/keq045
- Nichols, B. A., Bainton, D. F., & Farquhar, M. G. (1971). DIFFERENTIATION OF MONOCYTES : Origin, Nature, and Fate of Their Azurophil Granules. The Journal of Cell Biology, 50(2), 498–515.
- Sundman, E.A. et al. (2013). The Anti-inflammatory and Matrix Restorative Mechanisms of Platelet-Rich Plasma in Osteoarthritis. The American Journal of Sports Medicine.Vol 42, Issue 1, pp. 35 – 41
- Duarte, J. et al. Platelet-Rich Plasma: Regenerative Medicine: Sports Medicine, Orthopedic, and Recovery of Musculoskeletal Injuries. Springer Science & Business Media, Oct 29, 2013 pp 220
By now we have gained insight into the basics of Regenerative Medicine, such as where PRP and Stem Cells come from and their therapeutic applications for canine patients. It is generally understood that stem cells can be found in any tissue of the body. The two most common sources of stem cells for therapeutic applications are adipose tissue and bone marrow. A common misconception is that adipose derived stem cells provide a superior therapy versus bone marrow aspirate concentrate and that they are easier to collect and process. In this last segment of the Myth Buster Series, we will compare the two sources of stem cells, review their processing differences and determine if there really is a superior choice.
First, let’s consider how Adipose and Bone Marrow Derived Stem Cells are similar:
- They are both derived from the patient’s own body and are known as autologous adult-derived Mesenchymal stem cells
- Both can differentiate into cartilage, bone, tendon and ligament cell types.1
- They can treat certain similar indications with little to no clinical difference.2
- Both bone marrow and adipose derived stem cells can produce growth factors and anti-inflammatory proteins. These proteins have been shown to contribute to improved healing and reduced inflammation in injured tissues.3
- Both can be cultured to provide higher cell concentrations.
- There are commercially available systems to process either sample type.
- Collection of both Adipose tissue and Bone Marrow require anesthesia.
- Administration of either Adipose or Bone Marrow derived stem cells is typically done in combination with Platelet Rich Plasma.
- Fresh samples typically include a heterogenous mixture of several cell types.
Now let’s investigate how Adipose and Bone Marrow Derived Stem Cells are different:
♦ Time frame for processing
- Fresh Bone Marrow Aspirate Concentrate takes less than 30 minutes from collection to processing and can be done under one anesthetic episode.
- Fresh Adipose Derived Stem Cells take approximately 3-4 hours to process and require multiple anesthetic or sedative episodes.
♦ Processing requirements
- Fresh Bone Marrow Aspirate Concentrate involves collecting at least 25 mL of bone marrow from either the femur or humerus. It is then filtered and spun in a processing system for approximately 10 minutes. Once the spin is complete, the plasma is removed and 10% of total volume is collected.
- Fresh Adipose Derived Stem Cells involve taking approximately 20 grams of adipose under anesthesia, typically harvested from the falciform. The adipose is then mechanically and enzymatically disrupted to separate fat cells, blood cells and the Stromal Vascular Fraction.
- Stromal Vascular Fraction includes other cell types including white blood cells, fibroblasts, endothelial cells, hematopoietic stem cells and smooth muscle cells.
♦ Concentration of cells
- In a typical 25 mL collection of bone marrow aspirate, one can expect to have approximately 30,000 stem cells in 3 mL.
- A typical 20 gram collection of adipose (fresh) will yield 600,000 cells that are considered the Stromal Vascular Fraction.
- Please Note: There is little evidence in current research that suggests the ideal number of stem cells for treating certain conditions. In one such case, investigated in this peer reviewed paper by B. Carr, et. al., the small number of stem cells found in Bone Marrow Aspirate resulted in similar clinical effects compared to the higher concentration used from Adipose tissue. As our knowledge continues to evolve surrounding indications and specific protocols, these numbers may vary depending on what is being treated.
♦ Open vs. Closed System
- With Bone Marrow Aspiration, commercially available in-house systems are fully enclosed since the cells are collected via syringe and placed directly into concentrating devices.
- For Adipose processing, conical tubes are used for adipose digestion and processing, which is classified as an “open system”. This generally means that the samples are exposed to the outside environment which may affect the contents that are being processed. In academic and industry research facilities, it is typically recommended that samples processed utilizing open containers be placed in a fume hood to limit exposure to the surrounding environment.
♦ Equipment Necessary to Process Samples
- Processing Bone Marrow Concentrate requires a specialized centrifuge designed for concentration of the aspirate. Commercially available kits typically provide syringes, bone marrow collection needles, anticoagulant and concentrating devices.
- Processing Adipose Tissue requires a specialized centrifuge along with additional equipment including incubator water bath and agitator. Commercially available kits also provide syringes, anticoagulant, enzymes and concentrating devices/ processing tubes.
AND THE WINNER IS………………………Well, there really isn’t a winner or a loser in this case. Both Adipose and Bone Marrow Derived Stem Cells can be collected, processed and administered in the same day. Granted, there are differences in the processing times, cell concentrations and collection techniques, however, both therapies provide clinically effective results for similar indications. Deciding which tissue to collect stem cells from is dependent on personal preferences and training. There are numerous educational courses that provide hands-on instruction for either collection technique. If you are interested in learning bone marrow collection and processing, check out one of our upcoming Companion Regenerative University courses. The most important question to ask is “What is my goal for providing this therapy?”. If you answer that question, you may come out with your own Adipose vs. Bone Marrow Derived Stem Cell winner.
Stay tuned for our next blog which will investigate the role of White Blood Cells and their inclusion or exclusion in Platelet Rich Plasma!
References:
- The comparison of multilineage differentiation of bone marrow and adipose-derived mesenchymal stem cells. Xishan Zhu, Jing Du, Gang Liu. Clin Lab. 2012; 58(9-10): 897–903.
- Partial Cranial Cruciate Ligament Tears Treated with Stem Cell and Platelet-Rich Plasma Combination Therapy in 36 Dogs: A Retrospective Study. Canapp S.O. Jr, Leasure C.S., Cox K., Ibrahim V. and Carr B.J. (2016) Front. Vet. Sci. 3:112. doi: 10.3389/fvets.2016.00112
- Y.-M. Pers, M. Ruiz, D. Noël, C. Jorgensen, Mesenchymal stem cells for the management of inflammation in osteoarthritis: state of the art and perspectives, Osteoarthritis and Cartilage, Volume 23, Issue 11, November 2015, Pages 2027-2035, ISSN 1063-4584, http://dx.doi.org/10.1016/j.joca.2015.07.004.
With the growing area of regenerative medicine, it’s no surprise that there are dozens of systems available to process Platelet Rich Plasma (PRP). While the use of each system will result in a plasma product, the processing techniques, equipment and final sample differ quite drastically. In this installment of our Myth Buster series, we will take a closer look at the differences that one can expect to encounter when looking at PRP processing systems and how each of these components effects the PRP product.
Processing Techniques
There are three main methods by which Platelet Rich Plasma can be processed. These methods are:
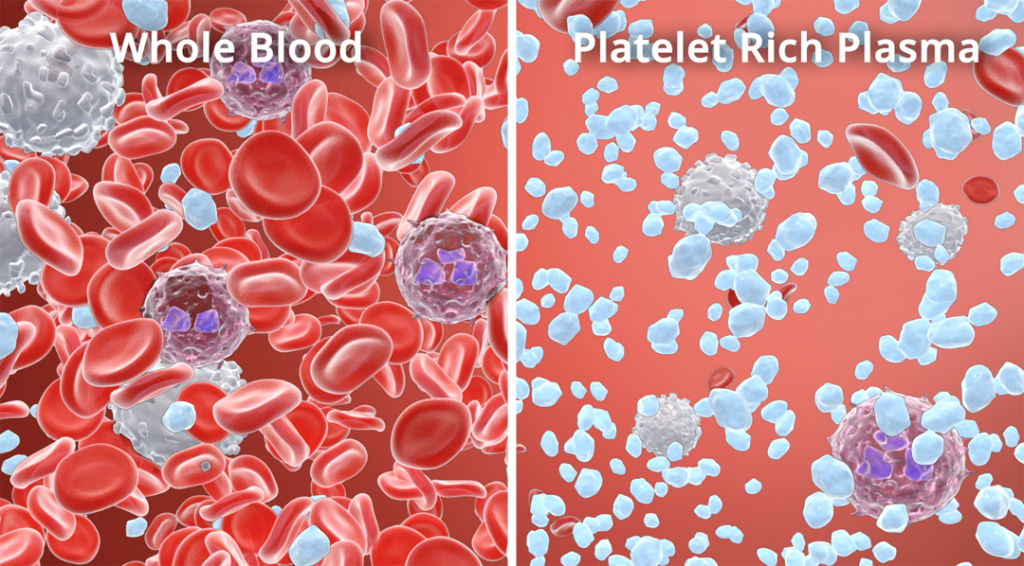
1. Centrifugation – This is the most common technique available, which involves using a centrifuge to separate the cell layers in whole blood or to pass the blood components through a gel separator (which is in the device prior to insertion of blood) to isolate the platelets from other cell types.
a.  Spinning without gel separator – When blood is spun at a high rate of speed for a period of time, the cellular components will separate according to their density within the container/tube. These cell layers can be visualized upon removal of the device as seen in the below picture. The three distinct layers of blood include the plasma layer, the platelet buffy coat and the red blood cell layer. The plasma and buffy coat can be collected and injected or the suspension can be placed in a second container for a second spin. The second spin in the process enables further concentration of the platelets, which as we discussed in our previous posts, is important for delivering a therapeutic concentration of platelets (between 3-7-fold concentration compared to circulating blood). A sample that is obtained by a single spin process will have a lower concentration of platelets, thus possibly resulting in a sub-optimal therapy.
Spinning without gel separator – When blood is spun at a high rate of speed for a period of time, the cellular components will separate according to their density within the container/tube. These cell layers can be visualized upon removal of the device as seen in the below picture. The three distinct layers of blood include the plasma layer, the platelet buffy coat and the red blood cell layer. The plasma and buffy coat can be collected and injected or the suspension can be placed in a second container for a second spin. The second spin in the process enables further concentration of the platelets, which as we discussed in our previous posts, is important for delivering a therapeutic concentration of platelets (between 3-7-fold concentration compared to circulating blood). A sample that is obtained by a single spin process will have a lower concentration of platelets, thus possibly resulting in a sub-optimal therapy.
b. Spinning with gel separator – Gel separators provide a physical gradient for blood to pass through resulting with the final product at the top of the tubes. Gel separators are typically used for isolating either plasma or serum, but have been developed to allow smaller cell types to remain in the final product. Unfortunately, the majority of products available that use gel separation produce a low concentration of platelets due to the small volume of blood being used (typically 8- 10 mL) as well as the poor capture of platelets in the final product.
2. Flow Cytometry - This method involves a highly specialized piece of equipment that utilizes the absorption of light by a cell and further separates the cells according to the refracting light. This process relies on blood flowing in a single layer suspension through a complex network of tubes, which can be further complicated if the sample begins to clot during the process. Flow cytometry is typically automated, which provides great convenience to the user, but the equipment may require additional set up (prior to processing) and upkeep to ensure proper calibration for processing samples.
3. Gravity and Reverse Osmosis – This method involves utilizing a specially designed blood containment system with a built-in filter. The filter’s purpose is to collect the platelets while allowing the other cells to pass through. Although this method is attractive from a space and equipment perspective, performance of these systems has shown to result in an increase of neutrophils which can be detrimental when injected into a joint.
Volume of Blood
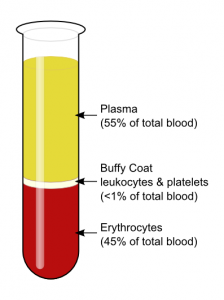 One of the biggest differences between PRP processing systems is the volume of blood that is required to obtain the PRP. Some systems require as low as 8 mL of whole blood, while other systems, such as the CRT system, require between 25-50 mL. What does this variation mean to you? If we look at typical blood composition, as depicted in the picture below, we will see that platelets make up less than 1% of the circulating blood. In order to have a therapeutic dose of platelets in the volume which is necessary for administration, a higher volume of blood is required for processing. For example, when using the CRT system, it is recommended to collect 50 mL of whole blood to produce 4-5 mL of PRP (with concentration of platelets between 3-7 fold). For systems that require the smaller whole blood volume with the same end product volume, the concentration of platelets will be below the recommended therapeutic threshold.
One of the biggest differences between PRP processing systems is the volume of blood that is required to obtain the PRP. Some systems require as low as 8 mL of whole blood, while other systems, such as the CRT system, require between 25-50 mL. What does this variation mean to you? If we look at typical blood composition, as depicted in the picture below, we will see that platelets make up less than 1% of the circulating blood. In order to have a therapeutic dose of platelets in the volume which is necessary for administration, a higher volume of blood is required for processing. For example, when using the CRT system, it is recommended to collect 50 mL of whole blood to produce 4-5 mL of PRP (with concentration of platelets between 3-7 fold). For systems that require the smaller whole blood volume with the same end product volume, the concentration of platelets will be below the recommended therapeutic threshold.
Sterility/ Exposure to Environment
When considering any product that will be administered intra-articularly or into areas of poor blood flow, it is imperative to ensure that the processing is done with aseptic technique. It is also important that the exposure of the sample to environmental factors is minimal to reduce the likelihood of contamination. The majority of systems available are considered to be closed systems in which the sample being processed has little to no contact with the outside environment. There are some processing systems available which utilize open tubes or require passing the blood through a needle into the containment device, which may introduce additional contaminants into the sample.
Time to Process- From Collection to Administration
Depending on the technique of isolating the platelets (centrifuge vs. flow cytometry vs. gravity filter), processing times vary greatly from just under 10 minutes to as much as 45 minutes! Some processing systems require activation of the platelets, which can take up to 45 minutes. Activating platelets, however, is not a necessary step, since the platelets will activate and release their stored growth factors once they are exposed to collagen in the joint/tissue. The Companion Regenerative Therapies System takes less than 15 minutes from blood collection to administration, making it a fast, in-house therapy that can be easily scheduled even in a busy hospital.
To learn more about Platelet Rich Plasma and how it works as a therapy, watch this short animation:
Stay tuned for our next blog post where we “bust” another regenerative medicine myth!